-
PROVIDERS
New MRD Medicare Coverage for Select Indications*
*When coverage criteria are met. Additional criteria and exceptions for coverage may apply.
-
LIFE SCIENCES
ENROLL NOW
Tempus’ patient-derived organoid screens
Evaluate the efficacy of your preclinical compounds using fixed organoid panels designed for diverse therapeutic applications -
PATIENTS
It's About Time
View the Tempus vision.
- RESOURCES
-
ABOUT US
View Job Postings
We’re looking for people who can change the world.
- INVESTORS
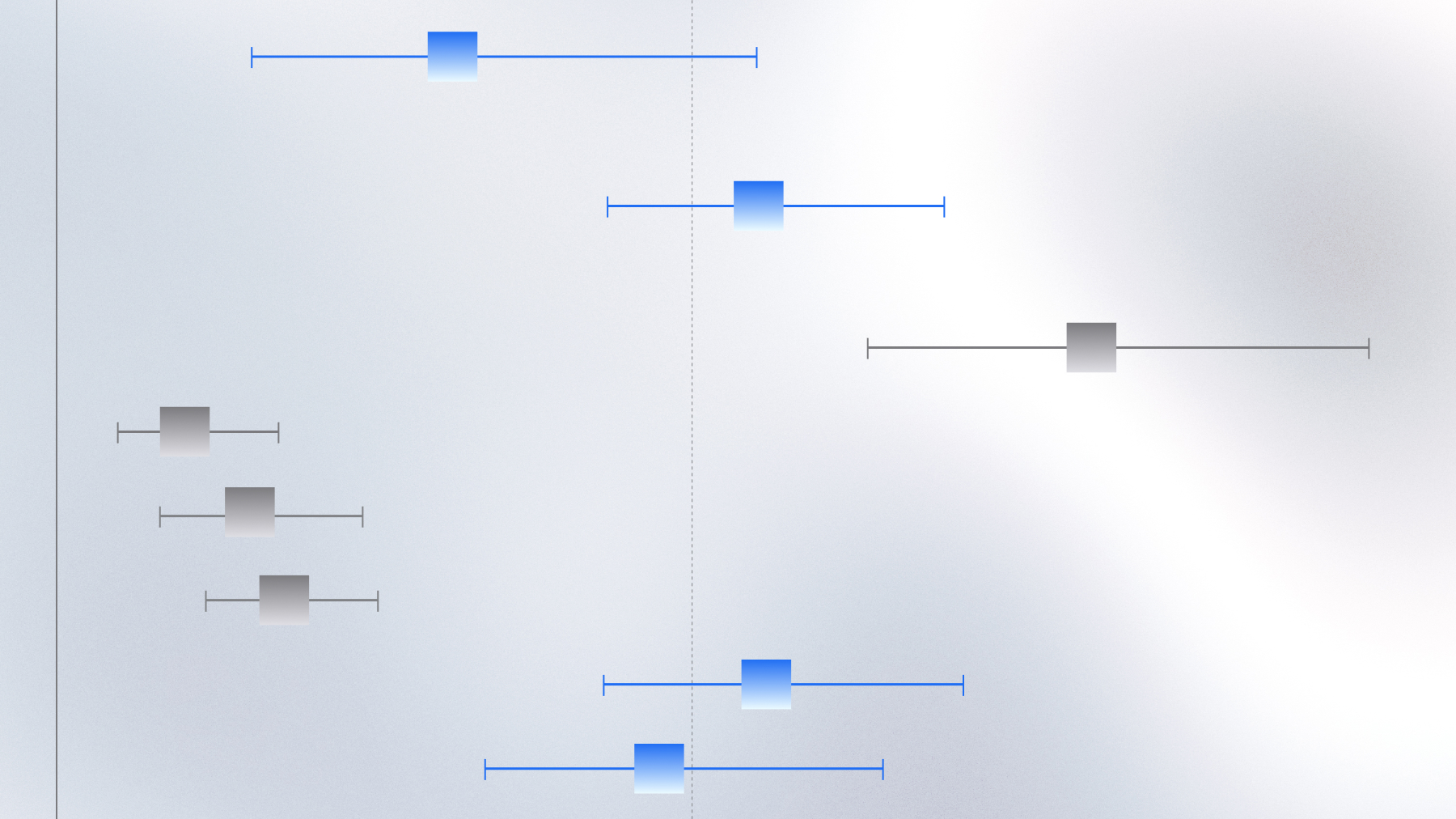
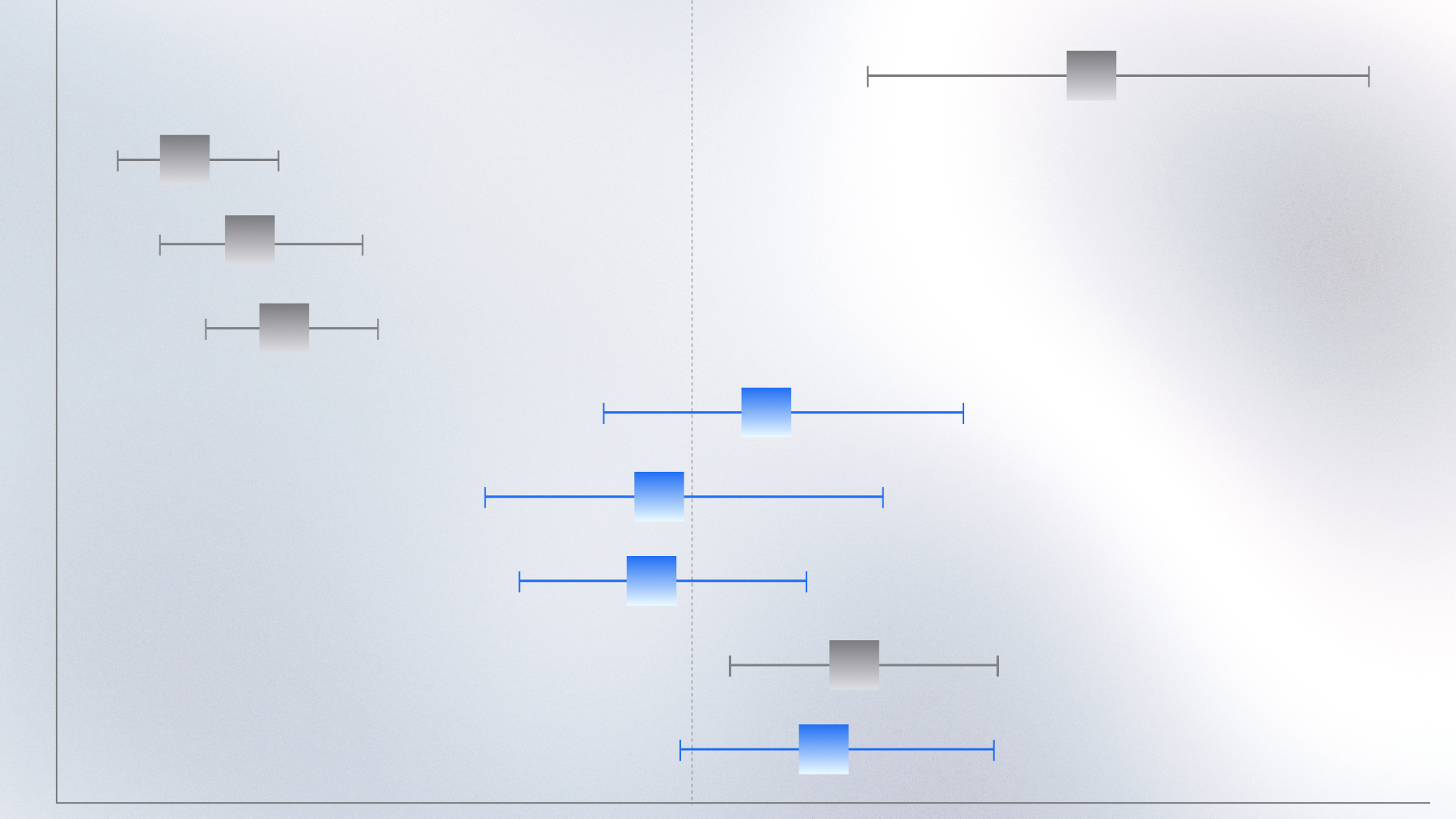
9p21 loss and low interferon expression predict poor ICI response in NSCLC
RWD analysis links combined 9p21 loss and low IFNK expression to ICI resistance in NSCLC
Contact us
Learn more about Tempus or explore more Lens research projects.