-
PROVIDERS
New MRD Medicare Coverage for Select Indications*
*When coverage criteria are met. Additional criteria and exceptions for coverage may apply.
-
LIFE SCIENCES
REGISTER NOW
UPCOMING WEBINAR
Driving enterprise value with RWD -
PATIENTS
It's About Time
View the Tempus vision.
- RESOURCES
-
ABOUT US
View Job Postings
We’re looking for people who can change the world.
- INVESTORS
08/13/2025
Q&A: How Mercy Health System uses AI to close care gaps in breast cancer
Experts from Mercy Health System discuss their implementation of Tempus Next, a care pathway intelligence platform, to support adherence to clinical guidelines and assist providers in delivering guideline-based care in a real-world setting.
Speakers
Jay Carlson, DO, MS
Medical Director, Oncology Service Line, Mercy Health Clinical Chair, Mercy Research

Molly Porter, MSN, FNP-BC
Nurse Practitioner, Mercy
Precision Medicine

Ezra Cohen, MD
Chief Medical Officer of Oncology, Tempus

Medical Director, Oncology Service Line, Mercy Health Clinical Chair, Mercy Research

Molly Porter, MSN, FNP-BC
Nurse Practitioner, Mercy
Precision Medicine

Ezra Cohen, MD
Chief Medical Officer of Oncology, Tempus

With breast cancer care evolving faster than ever, providers face a critical challenge: how can they make sure that every eligible patient benefits from the latest guideline-directed care? For busy providers the question becomes how to bridge the gap between complex, ever-evolving guidelines and the delivery of personalized care to each patient.
Mercy Health System tackled this challenge head-on by implementing Tempus Next, a care pathway intelligence platform that uses AI to help providers identify and address care gaps. In a recent webinar, we went behind the scenes with leaders from Mercy to discuss their firsthand experience – from initial implementation to their experience integrating AI-enabled tools into their clinical workflow.
The discussion features Dr. Jay Carlson, Medical Director for the Oncology Service Line at Mercy Health, and Molly Porter (MSN, FNP-BC), a Nurse Practitioner with Mercy Precision Medicine. They are joined by moderator Dr. Ezra Cohen, Chief Medical Officer of Oncology at Tempus.
Dr. Ezra Cohen: What are the biggest challenges in applying clinical guidelines at a large health system like Mercy? |
Dr. Jay Carlson: The challenges fall into two main categories: provider-specific and system-specific. For providers, time is their most precious commodity. They are well-intentioned but can get overwhelmed by the sheer volume of patients and daily tasks. At a system level, it is difficult to deploy the necessary checks and balances at scale across our entire network, which includes 80 oncology providers across multiple states. |
Dr. Ezra Cohen: Why did Mercy Health choose to implement an AI-powered platform like Tempus Next, and why start with breast cancer? |
|
Dr. Jay Carlson: We chose to implement Tempus Next because it fit seamlessly into our existing infrastructure. Mercy had already established a centralized Precision Medicine department, so the platform folded into that workflow without requiring a significant additional lift.We started with breast cancer for a few key reasons. First, the NCCN guidelines for breast cancer are updated so frequently that it is difficult for providers to stay current. The complexity of these guidelines, combined with the straightforward approach Tempus offered, made it an ideal starting point for our initiative.
|
Dr. Ezra Cohen: How does the Tempus Next platform work in your day-to-day clinical workflow? |
| Molly Porter, MSN, FNP-BC: Our precision medicine team uses a centralized workflow, which has been critical to our success. My team and I check the Tempus portal once a week to identify any patients with care gaps. We then perform a brief chart review and send a secure message to the patient’s oncologist using specific templates. This process is designed to be as non-disruptive as possible. The portal is very straightforward to use, and the ability to customize it to our needs has made the process smooth and efficient. |
Dr. Ezra Cohen: What have the results been since implementing the platform? |
Molly Porter, MSN, FNP-BC: In the first five months, we identified 26 patients with a gap in somatic profiling for breast cancer. We contacted the physicians for 11 of those patients who were candidates for testing but had not yet received it.
Dr. Jay Carlson: An important component is that the number of care gaps we identify is decreasing over time. Providers are becoming more aware and sensitive to the guidelines, so they are ordering the appropriate testing upfront. The program serves as a check and balance, but we are also educating providers and changing behavior, which was a key goal. |
Dr. Ezra Cohen: Can you share a success story that illustrates the platform’s impact? |
| Molly Porter, MSN, FNP-BC: We had a situation where the platform helped us identify that a test was not being ordered correctly by a provider. This became a teaching moment for the oncologist and their team. That correction doesn’t just impact that one patient; it has a downstream effect that improves care for all of their future patients. That is a true success. |
Dr. Ezra Cohen: How do providers react when an AI recommendation differs from their clinical judgment? |
| Dr. Jay Carlson: We honor the autonomy of the individual provider. The platform provides a notification and a recommendation based on clinical guidelines, but the final decision on whether to order a test or follow a specific therapy rests with the provider and their patient. The tool is there to support their decision-making, not replace it. |
Dr. Ezra Cohen: How does a platform like this help address health disparities in cancer care? |
| Dr. Jay Carlson: The platform is objective. When it identifies a care gap, it is based purely on the data—the cancer type, the stage, and the recommended testing guidelines. It does not factor in other information that can introduce bias. We communicate the findings to the providers, and they can leverage their own judgment, but at least they are made aware of the care gap for every patient who meets the criteria. This helps ensure everyone that is eligible is considered for the same high standard of guideline directed care. |
Dr. Ezra Cohen: What does the future of AI in oncology care look like from your perspective? |
|
Molly Porter, MSN, FNP-BC: As AI evolves, the goal is to find the least disruptive way to close care gaps and do the right thing for the patient. Continuing to use a centralized team model will be key to making sure we can support providers without adding to their workload.Dr. Jay Carlson: I think the only thing we are waiting for is the next cancer type. We have it for lung and breast cancer, and we are ready for prostate, colorectal, and others. These tools are helping our providers deliver guideline-based care, and they are here to stay.
|
| To learn more about Tempus’ role in advancing precision medicine, we invite you to watch the webinar recording. For in-depth demonstrations of our AI-enabled applications, contact us here. |
-
11/11/2025
A new era of biopharma R&D: The TechBio revolution—realities and the next frontier
Join Tempus and Recursion leaders to explore their strategic TechBio partnership. Learn how they use AI and supercomputing with petabytes of data to accelerate drug discovery and development. See the impact on biopharma R&D's future.
Watch replay -
11/14/2025
Validating a novel target and informing trial design for a first-in-class therapeutic
Discover how a biopharma company used Tempus’ de-identified multimodal data to support validation of a novel target and inform trial design for a first-in-class therapeutic.
Read more -
11/14/2025
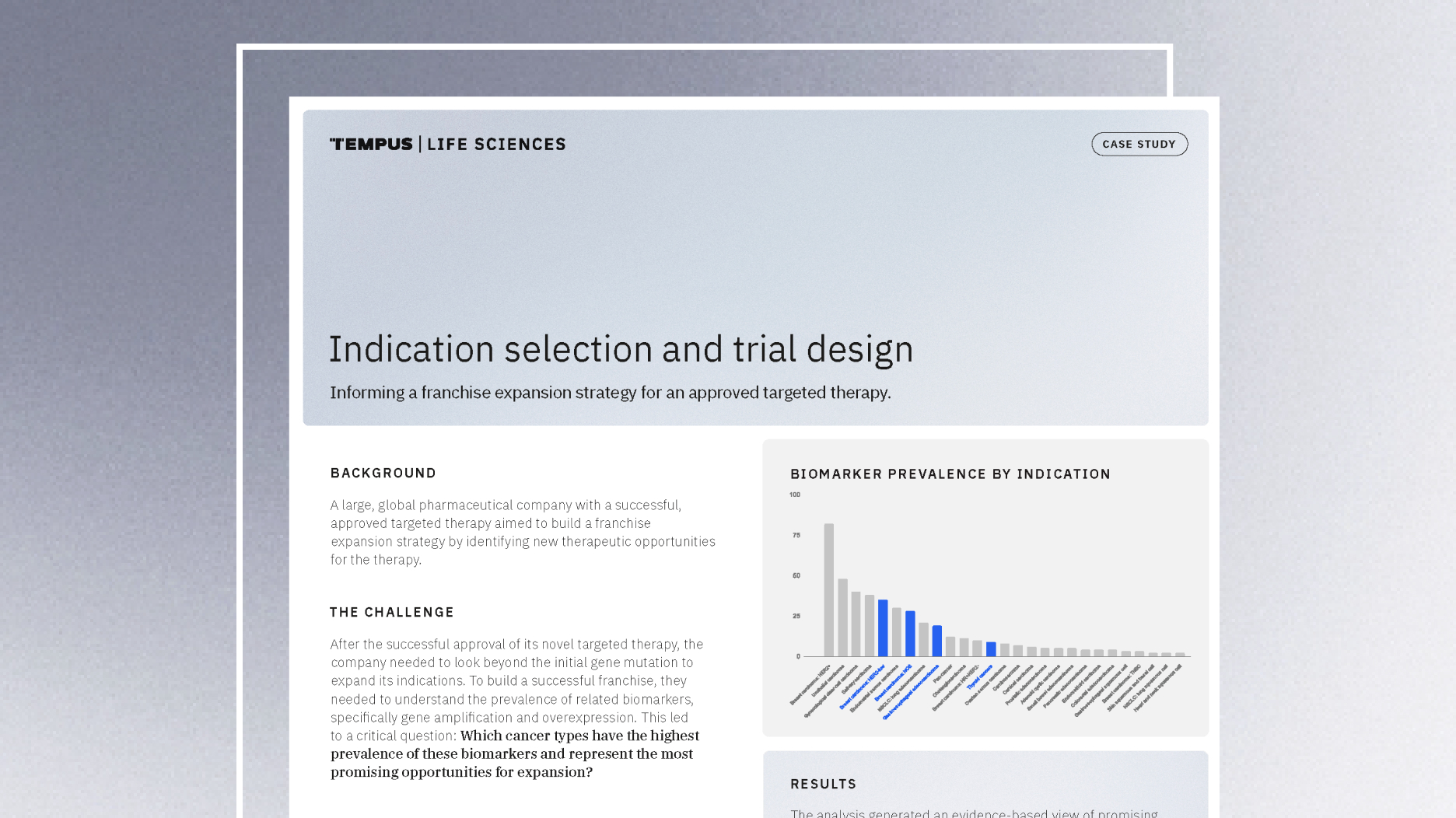
Guiding indication expansion with multimodal real-world data
Discover how a biopharma company used Tempus’ multimodal real-world data to guide its indication expansion strategy. See how our analysis of biomarker prevalence helped them identify new opportunities, prioritize R&D, and inform future trial design.
Read more